Abstract
Background: Mutations in the NPM1 gene are among the most common genetic alterations in patients with acute myeloid leukemia (AML). NPM1 mutations predominantly occur in patients with normal or intermediate-risk abnormal cytogenetics, and define a distinct subgroup of AML patients recognized in the 2016 WHO classification. Overall, mutated NPM1 associates with favorable response to induction chemotherapy and relatively favorable overall survival. However, this prognostic impact is modulated by the presence of other gene mutations including FLT3 internal tandem duplications (ITD) and DNMT3A mutations. Recently, Patel and colleagues reported that a high variant allele frequency (VAF) of mutated NPM1 at the time of initial diagnosis associates with unfavorable outcomes in de novo AML (Blood 131:2816-25). This interesting and unexpected observation prompted us to investigate the association between NPM1 VAF and outcomes in a large AML patient cohort.
Patients and Methods: We studied NPM1 mutated AML patients who had been enrolled on two successive multicenter phase III trials of the German AML Cooperative Group (AML-CG 1999, NCT00266136; AML-CG 2008, NCT01382147) and genetically characterized by amplicon-based targeted next-generation sequencing (NGS, Agilent Haloplex; Metzeler et al., Blood 128:686-98 and unpublished data). All patients had received induction chemotherapy containing cytarabine with either daunorubicin plus thioguanine or mitoxantrone. The minimum VAF for calling of insertion/deletion variants was 0.05, and samples with NPM1 coverage <100-fold (n=17) were excluded. FLT3 internal tandem duplication (ITD) status and FLT3 ITD-to-wild type allelic ratio were determined by PCR and fragment analysis from gDNA.
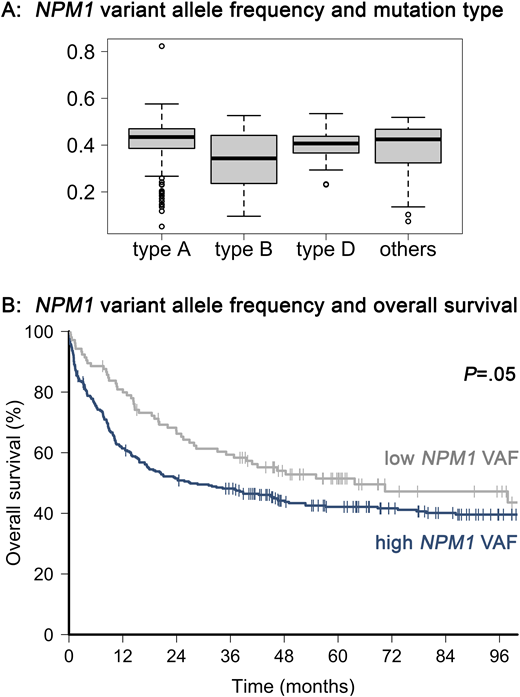
Results: We identified 417 NPM1-mutated patients (type A mutations, 316; type B, 28; type D, 35; and other types, 38). Median patient age was 56 years (range, 19 - 86 years), and 31/414 patients (7.5%) with cytogenetic data had abnormal karyotypes. The median NPM1 VAF was 0.43 (range, 0.05 to 1.0). Type A NPM1 mutations had significantly higher VAFs than non-type A mutations (median, 0.43 vs. 0.41; P=.0002), while type B mutations had lower VAFs than non-type B mutations (median, 0.34 vs. 0.43; P=.0025) (Figure A). Age or karyotype did not associate with NPM1 VAF.
NPM1 VAF, as a continuous variable, did not associate with response to induction chemotherapy (P=.6) or relapse-free survival (P=.22). A higher NPM1 VAF did, however, associate with shorter OS (hazard ratio for an increase in NPM1 VAF equal to the interquartile range, 1.14; 95% confidence interval, 1.00-1.30; P=.049). In particular, patients in the lowest quartile of NPM1 allele burden ('low NPM1 VAF') had longer OS than patients with allele burdens above the 25th percentile ('high NPM1 VAF') (median OS, 63.7 vs. 27.0 months; 5-year OS, 51% vs 42%; P=.05; Figure B).
Patients with high NPM1 VAF had higher leukocyte counts (median, 46000/µl vs. 9300/µl; P<.0001) and bone marrow blast percentages (median, 85% vs. 80%; P=.0004) than patients with low NPM1 VAF. On the genetic level, patients with high NPM1 VAF more frequently had concomitant FLT3-ITD (47% vs. 37%; P=.07), and particularly FLT3-ITD with a high (≥0.5) mutant-to-wild type ratio (33% vs. 17%; P=.007), compared to patients with low NPM1 VAF. DNMT3A co-mutation was also more frequent in patients with high vs. low NPM1 VAF (63% vs. 46%; P=.002). In multivariable analyses adjusting for FLT3-ITD allelic ratio and/or DNMT3A mutation status, only the latter genetic alterations but not NPM1 VAF remained associated with OS.
Conclusion: Our study confirms the recent report that adult AML patients with high NPM1 mutant allele burden have shorter survival. In our cohort, however, higher NPM1 VAF also associated with higher leukocyte counts and marrow blast percentage, and with prognostically adverse FLT3-ITD and DNMT3A mutations. After adjusting for these confounders, NPM1 allelic burden did not independently predict survival in our analysis. We therefore suspect that high NPM1 VAF may be a surrogate marker of highly proliferative AML subsets, for example those with high allelic ratio FLT3-ITD, rather than a novel independent prognostic factor.
Prassek:Jannsen: Other: Travel support; Celgene: Other: Travel support. Subklewe:Roche: Consultancy, Research Funding; Gilead: Consultancy, Honoraria, Research Funding; Amgen: Consultancy, Honoraria, Research Funding; Pfizer: Consultancy, Honoraria; Celgene: Consultancy, Honoraria. Hiddemann:Janssen: Consultancy, Honoraria, Membership on an entity's Board of Directors or advisory committees, Research Funding; F. Hoffman-La Roche: Consultancy, Honoraria, Membership on an entity's Board of Directors or advisory committees, Research Funding; Bayer: Consultancy, Research Funding; Celgene: Consultancy, Honoraria, Membership on an entity's Board of Directors or advisory committees, Research Funding. Metzeler:Celgene: Consultancy, Research Funding; Novartis: Consultancy.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal